The Medical Definition of Telemedicine: Bridging Healthcare Across Distances
The Medical Definition of Telemedicine: Bridging Healthcare Across Distances
Telemedicine, in its most precise medial definition, is the delivery of clinical healthcare services—diagnosis, treatment, monitoring, and consultation—through digital communication technologies, enabling real-time or asynchronous patient-provider interaction irrespective of geographic separation. Far beyond simple video calls, telemedicine integrates secure platforms, remote diagnostic tools, and electronic health records to replicate, and in many cases enhance, the experience and efficacy of in-person care. As defined by the World Health Organization (WHO), telemedicine “uses telecommunications technology to provide medical care from a distance,” emphasizing its role in overcoming barriers to access.
Rooted in history since early 20th-century radio consultations, modern telemedicine has evolved into a sophisticated healthcare modality supported by high-resolution imaging, wearable biosensors, and cloud-based data platforms. The core mechanism revolves around connectivity: patients communicate with clinicians via encrypted video, transmit health data in real time, and receive clinical decisions ranging from acute interventions to chronic disease management.
Types and Technological Foundations of Telemedicine
Telemedicine encompasses diverse modalities, each tailored to specific clinical needs and technological capabilities.Categorized by interaction style, the main forms include: - **Synchronous consultation**: Real-time video or audio sessions where patient and provider interact live, mimicking face-to-face visits. This format dominates current practice and relies on stable broadband connectivity and HIPAA-compliant software. - **Asynchronous (store-and-forward)**: Medical data—such as radiology images, dermatology photos, or lab results—are securely transmitted to providers who review them at a later time.
This method enables specialist time-zone flexibility and supports high-accuracy diagnostics. - **Remote patient monitoring (RPM)**: Continuous or periodic collection of physiological data via wearable devices and home health monitors. RPM captures vital signs like blood pressure, glucose levels, or heart rate, allowing proactive intervention in conditions such as diabetes or heart failure.
- **Mobile health (mHealth)**: Uses smartphones and apps for health management, including symptom tracking, appointment reminders, and teletherapy. This modality integrates seamlessly into daily life, expanding reach to underserved populations. These types are underpinned by a robust technological infrastructure: cloud computing stores health data securely; AI-assisted diagnostic tools enhance accuracy; and interoperable electronic health records (EHRs) ensure seamless information flow between providers.
As the American Medical Association notes, telemedicine “reformulates care delivery by prioritizing accessibility without sacrificing clinical rigor.”
Telemedicine’s scope extends beyond routine check-ups to emergency triage, mental health support, emergency mental health responses, and post-operative follow-ups. During the global pandemic, its adoption surged, with telehealth visits increasing by over 380% in 2020 alone, according to the CDC. This rapid expansion validated telemedicine not as a temporary fix but as a permanent pillar of modern healthcare delivery.
Applications Across Clinical Specialties Telemedicine’s adaptability makes it indispensable across medical domains:


Related Post
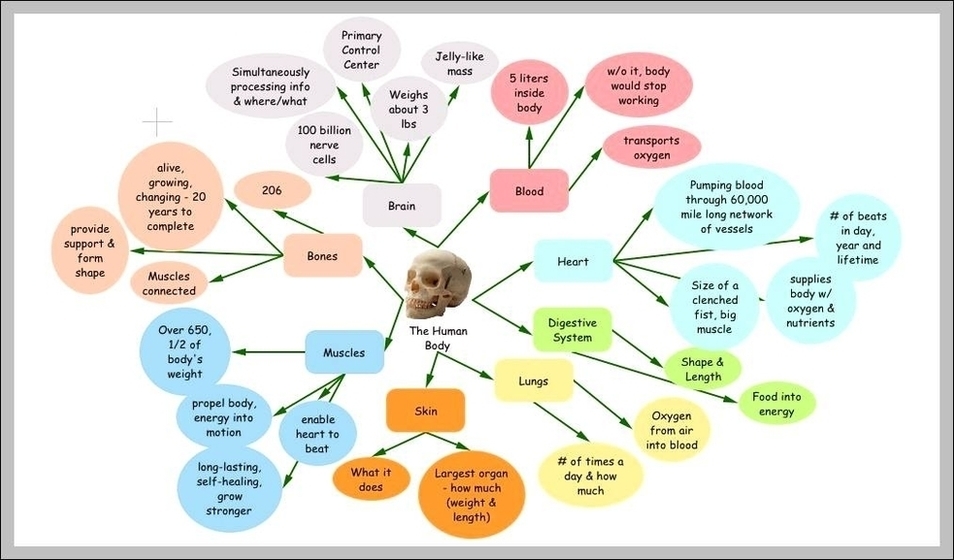
Medial Definition Anatomy: The Master Map of the Human Body

Ayam Wiring Kuning Asli Tembus Luar Biasa: The Timeless Craft Behind Bangkok’s Rural Koleksi
Gary ODonoghue BBC News Bio Wiki Age Height Family Wife Eyes Salary and Net Worth

Cast Despicable Me: How Minions Transcended Animation to Become Global Cultural Icons

