Umaga Cause of Death: Unraveling the Silent Epidemic Behind Global Mortality
Umaga Cause of Death: Unraveling the Silent Epidemic Behind Global Mortality
When analyzing global health trends, one critical metric stands out above all: Umaga Cause of Death. This phrase refers not to a single illness, but to a complex, often hidden contributor to premature mortality—one that demands urgent attention in public health discourse. Each suicide, overdose, accident, or chronic disease-related demise carries deeper systemic forces, from mental health crises to socioeconomic neglect.
Understanding the true cause of death—beyond textbook diagnoses—is essential for crafting effective prevention strategies and saving millions of lives worldwide.
Umaga Cause of Death encompasses more than a clinical label; it represents the culmination of biological, psychological, environmental, and social stressors that converge at the moment of fatal outcome. According to the World Health Organization (WHO), unintentional injuries—such as road traffic accidents, falls, and poisonings—rank among the leading causes, collectively responsible for nearly 4.7 million deaths annually.
Yet these figures mask a broader reality: mental health disorders, particularly suicide, account for a staggering 17% of global deaths, making suicide the fourth leading cause of death among 15–29-year-olds worldwide.
Unintentional injuries remain a dominant force in premature mortality, with nearly 3.6 million deaths per year attributed to road traffic injuries alone. Each incident is a preventable tragedy shaped by infrastructure design, road safety regulations, and behavioral choices. In low- and middle-income countries, inconsistent access to emergency care significantly increases fatality rates.
As Dr. Tedros Adhanom Ghebreyesus, WHO Director-General, noted: “Every death from accident is a call for stronger policies—safer roads, better urban planning, and accessible healthcare.” Transportation safety campaigns have proven effective; for example, mandatory helmet laws in Vietnam reduced motorcycle fatalities by 40% over a decade, demonstrating that targeted interventions save lives.
Suicide, another critical facet of Umaga Cause of Death, reveals profound societal and psychological undercurrents. Unlike acute physical illnesses, suicide often stems from prolonged mental health struggles—depression, trauma, isolation, or even economic despair—yet remains shrouded in stigma and silence.
The WHO emphasizes that “50% of suicide deaths occur before age 50,” with middle-aged adults especially vulnerable due to job loss, relationship breakdowns, or untreated mental disorders. Public health experts stress that suicide is not a personal failure but a public health emergency requiring accessible mental health services, crisis hotlines, and community support networks. Countries like Australia have pioneered national suicide prevention strategies, combining school-based education with culturally sensitive mental health outreach—resulting in measurable declines in self-harm incidents over the past decade.
Chronic and degenerative diseases, though often associated with older age, also fall under Umaga Cause of Death, driven heavily by modifiable lifestyle and environmental factors.
Cardiovascular disease, cancer, diabetes, and respiratory illnesses collectively claim over 18 million lives annually. Smoking, tobacco use, unhealthy diets, and physical inactivity amplify risk, but access to early screening and treatment remains uneven. In sub-Saharan Africa, late-stage cancer diagnoses are common, due in part to limited diagnostic infrastructure—highlighting how geography and poverty compound mortality risks.
Conversely, nations with robust primary healthcare systems—such as Japan—report lower rates of preventable deaths through widespread vaccination, cancer screening, and public education on healthy living.
Undermine the clarity of Umaga Cause of Death by recognizing its multidimensional nature: no single statistic tells the full story. Demographic variables—age, gender, socioeconomic status—profoundly influence risk. For instance, men die from preventable causes at nearly twice the rate of women globally, with men 2.3 times more likely to die by suicide, while women experience higher rates of substance overdose-related death.
These disparities reflect gender norms, occupational hazards, and differential access to care. Similarly, rural populations face unique challenges: limited hospital access, scarce mental health professionals, and transportation barriers increase mortality risks across all categories.
Emerging data also highlight the growing impact of environmental and climate-related causes. Air pollution contributes to an estimated 6.7 million premature deaths annually, with fine particulate matter infiltrating lungs and bloodstream to trigger heart attacks, strokes, and lung cancer.
Natural disasters—intensified by climate change—displace communities, disrupt medical care, and increase injury and disease amid squalor. Heatwaves, now more frequent and severe, alone killed over 60,000 people in Europe in 2022, underscoring the urgent need to integrate climate resilience into public health planning.
The true power of understanding Umaga Cause of Death lies in translating data into action. While mortality statistics quantify loss, they also serve as blueprints for intervention.
Public health initiatives grounded in epidemiological evidence—such as expanding opioid prescription monitoring, funding mental health crisis centers, enforcing road safety laws, or reducing tobacco use—have proven transformative. In Portugal, decriminalizing drug addiction shifted focus from punishment to treatment, resulting in steep drops in overdose deaths and HIV transmission. These examples prove that behind every number is a life, a family, and an opportunity to prevent future loss.
Preliminary analyses confirm that many deaths classified under Umaga Cause of Death are not inevitable—a leading cause of death in one population may be preventable in another.
The gap hinges on societal commitment, resource allocation, and political will. Investing in education, healthcare infrastructure, mental health parity, and safe urban environments not only reduces preventable mortality but strengthens community resilience. As Dr.
Maria Van Kerkhove, WHO’s Technical Lead for COVID-19, puts it: “Every death is a story. To change the narrative, we must understand the causes—and act with urgency.”
In essence, Umaga Cause of Death is more than a measure of mortality—it is a mirror reflecting societal strengths and vulnerabilities. By confronting underlying risk factors through informed policy, compassionate care, and global cooperation, the world can reframe premature loss as a solvable challenge.
Each preventable death is a warning call; every effective intervention, a testament to human ingenuity. The path forward demands not just data, but decisive action—beginning with the urgent, unignorable truth of who, why, and how we die.



Related Post

What’s the Time in Brazil? The Complete Guide to Brazil Time Now and Across Its Regions

Top Russian Universities Ranked: Your Ultimate Guide to the Elite Academic Powerhouses of Russia
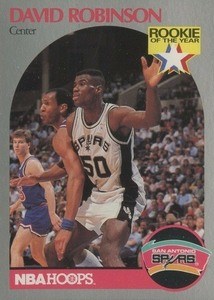
90–91 NBA Hoops Cards: The Legacy, Design, and Cultural Impact of a Defining Era in Hoop History