OCC Bacteria In Urine: Understanding The Results
The presence of OCC (Enterobacteriaceae) bacteria in urinary samples remains one of the most widely referenced indicators in clinical microbiology, offering critical insights into urinary tract health. While often trivialized in routine testing, laboratory results indicating OCC in urine signal more than just contamination—they reveal potential microbial encroachment, possible infection, or underlying urinary system dysfunction. Understanding what these findings mean, how they are interpreted, and what steps follow empowers patients and providers alike to respond effectively to this common yet complex indicator.
The Microbial Story Behind OCC in Urine
OCC, short for *Enterobacteriaceae*, is a family of gram-negative bacteria typically resident in the gastrointestinal tract, particularly the colon.Under normal circumstances, barriers such as adequate hydration and urine flow prevent significant bacterial migration into the urinary system. When OCC is detected in urine—especially in quantitative samples indicating a count exceeding 10 colony-forming units per milliliter (CFU/mL)—it suggests an interface where microbial ecology has shifted. “This presence isn’t inherently pathological,” explains Dr.
Sarah Lin, a clinical microbiologist specializing in urinary diagnostics. “But it marks the presence of microbes outside their usual niche—raising questions about exposure, hygiene, or infection.” Such organisms may include *Escherichia coli*, *Klebsiella pneumoniae*, and *Proteus mirabilis*, each carrying distinct clinical implications depending on context, patient health status, and bacteriomycology.
Quantification and context define the significance of OCC findings.
The clinical interpretation of OCC results heavily depends on quantitative thresholds and patient-specific factors.Urine microbiology is not judged solely on presence but on load,徛徛
recognizing whether it represents transient, incidental colonization or a harbinger of infection. A key benchmark in clinical guidelines is the distinction between recreational contamination and abnormal bacteriuria. Recreational OCC—detected in healthy individuals without symptoms—may arise from fecal-urinary tract overlap, poor hygiene, or diagnostic artifact.
These findings, while common, rarely warrant treatment unless recurrent or symptomatic. In contrast, persistent or elevated counts, particularly when accompanied by dysuria, fever, or flank pain, signal viable pathogenic invasion. Here, OCC serves as a clue pointing toward upper urinary tract involvement or systemic infection requiring targeted intervention.
Factors influencing bacterial detection extend beyond morphology, encompassing sample collection, storage, and regional microbial prevalence.
Mid-stream clean-catch specimens drastically reduce false positives by minimizing gastrointestinal cross-contamination, a caveat clinicians stress frequently. Contaminated samples from catheterized or perineal procedures inflate background flora counts, potentially misleading initial assessment. “Misinterpretation often stems from ignoring sample integrity and patient context,” warns Dr.
Marcelle DuVignes, a urologist with expertise in urinary diagnostics. “A patient with a single low count post-catheterization warrants observation, not antibiotic initiation. But the same level in a woman with new onset of pelvic discomfort demands thorough evaluation.”
Interpreting OCC results also benefits from integrating patient history and risk profiling.
Individuals with diabetes, immunodeficiency, renal abnormalities, or recent urinary tract instrumentation face heightened susceptibility to microbial colonization and sequelae. Recurrent episodes, defined as multiple detections across different specimens, often necessitate longer diagnostic follow-up—including urine culture and imaging—beyond routine quantification. \begin{itemize>
Brisk bacterial colonization correlates with urine pH and mucosal changes; clinicians tailor screening accordingly.
Persistent OCC post-catheter insertion signals biofilm formation or device-related infection risk.
From diagnostic pathways to treatment paradigms, OCC results shape clinical decision-making across care settings.
Initial steps typically involve repeat sterile mid-stream urine collection to confirm initial findings. Microbiologic culture, ideally with extended incubation for fastidious organisms like *Proteus* or *Enterobacteriaceae* variants, identifies species and antibiotic sensitivity—critical for precision therapy. “Culture remains the gold standard,” DuVignes notes.
“It transforms a numerical positive into a diagnosisable condition—whether a colonization event needing monitoring or an active infection demanding antibiotics.” For many patients, this distinction determines treatment necessity. Low-level, transient OCC may resolve resolvently with hydration alone; moderate loads with symptoms justify targeted antibiotics. Critical cases—investigations of pyelonephritis, sepsis, or obstructive pathology—require urgent intervention beyond oral therapy.
Prevention and patient education further anchor effective management. Hydration maintains dilute urine, minimizing bacterial adherence. Proper hygiene, delayed wiping after defecation, and timely catheter removal reduce friction points for microbial translocation.
Awareness empowers patients to recognize warning signs: burning urination, cloudy output, or shifting symptom patterns—prompting early testing rather than self-diagnosis.
OCC findings in urine, though routine, crystallize a complex microbial dialogue between patient, environment, and immune response. They are not simple positives or negatives but nuanced indicators demanding clinical context, patient history, and targeted action.
Misinterpretation risks both overtreatment and missed infections—making accurate understanding not just informative, but essential. As diagnostic microbiology advances, integrating OCC results with molecular profiling and patient-specific data promises even finer clinical insight, transforming routine samples into vital windows of health insight.
In summary, OCC in urine is a critical yet context-dependent marker, guiding diagnosis, treatment, and prevention with precision honed through scientific rigor and clinical experience.
Understanding its significance enables proactive, responsible care—one test at a time.




Related Post

Exploring Vids: How AI, Immersion, and Audience Behavior Are Rewriting the Rules of Video Content
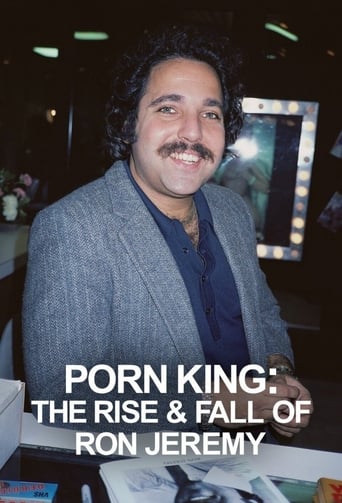
Ron Jeremy News: Inside the Controversial Career and Cultural Impact of a Erotic Icon
Unlock Your Health Potential with Ambetter Rewards: Earn Value While Investing in Your Well-Being

