Medical Certificate Forms: The Silent Gateway to Care, Compliance, and Patient Safety
Medical Certificate Forms: The Silent Gateway to Care, Compliance, and Patient Safety
From routine workplace absences to urgent medical deferrals, medical certificate forms serve as critical touchpoints between healthcare providers and institutions—legal records, clinical validations, and frontline safeguards rolled into one. These documents are far more than bureaucratic necessities; they are vital tools in maintaining continuity of care, protecting workplace health policies, and ensuring that medical judgment guides patient outcomes rather than guesswork. The formal role of a medical certificate form extends beyond simply confirming illness.
Defined by legal, occupational, and healthcare standards, these forms document diagnostic assessments, treatment plans, disability status, or fitness to work. They act as official proof of medical condition when employers, insurers, or care coordinators require objective documentation. “A well-completed medical certificate is not just a form—it’s a formal statement of a patient’s current health status,” notes Dr.
Elena Torres, a physician specializing in occupational health. “It affects return-to-work decisions, eligibility for disability support, and even public safety protocols.”
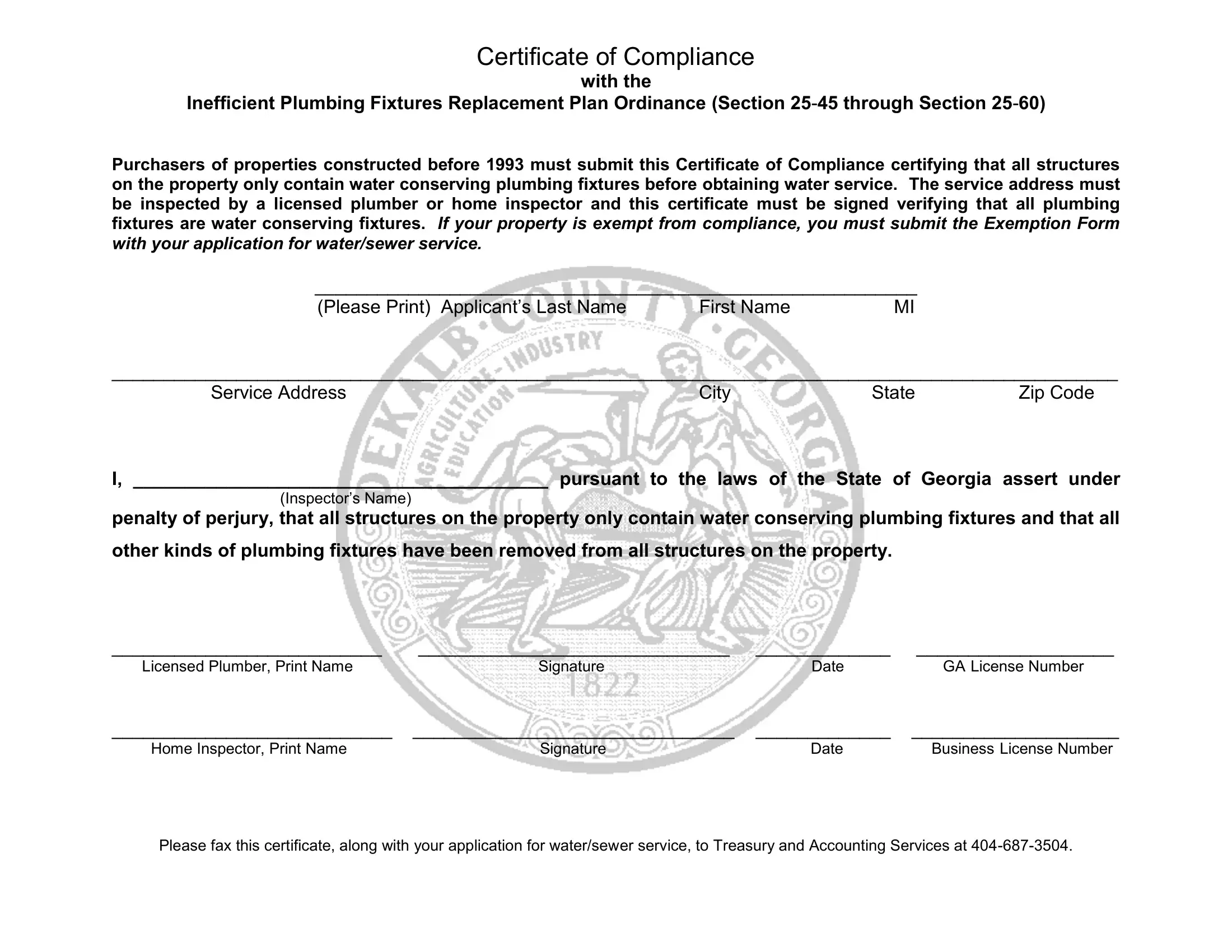
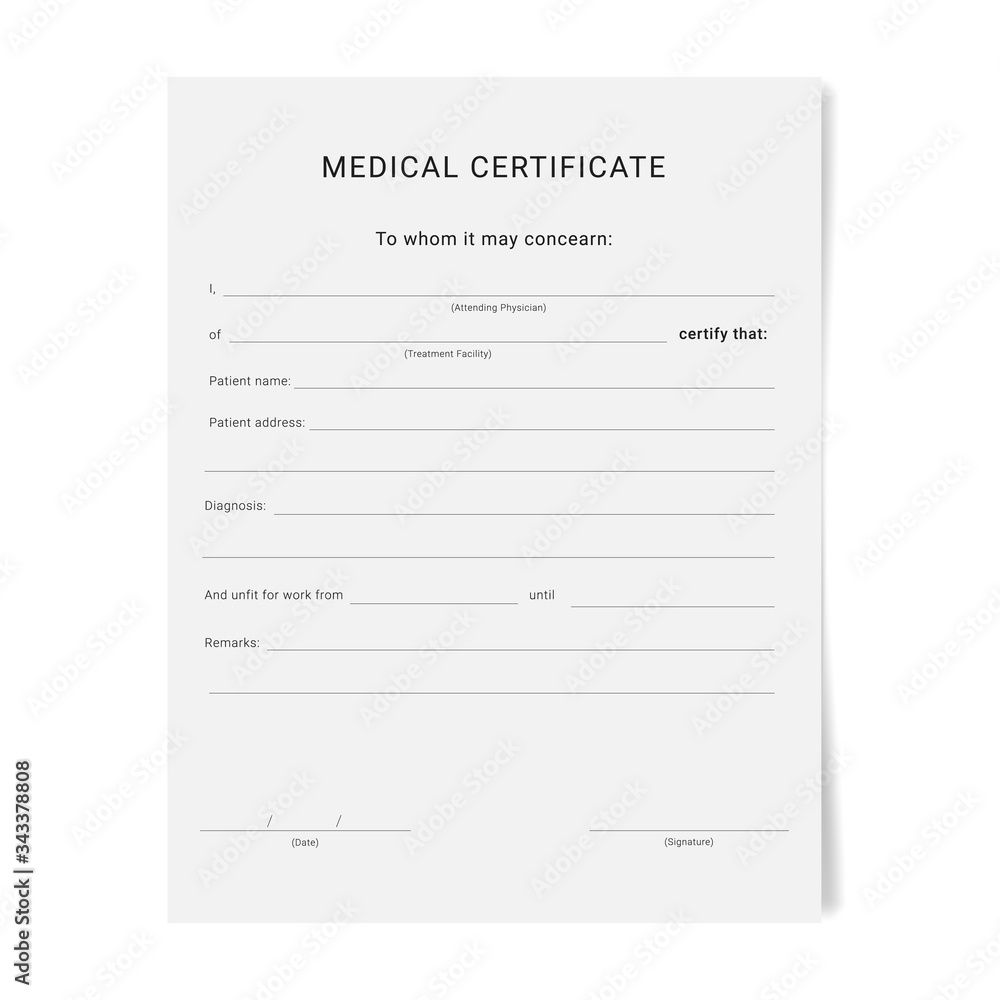
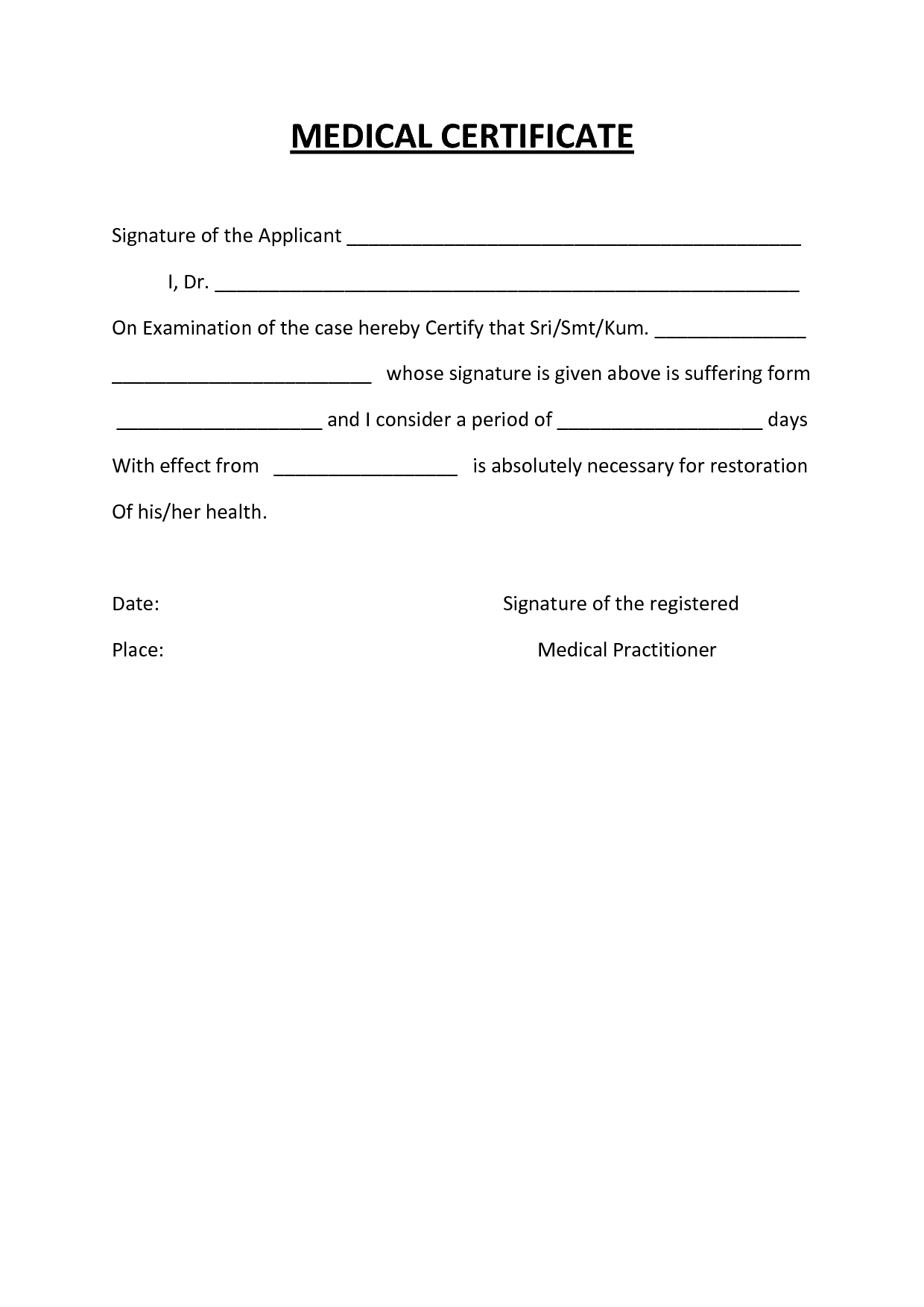
Medical certificate forms vary by context: workplace injury reports, school absence records under disability accommodations, and hospital discharge summaries all serve distinct purposes. For instance, a statutory occupational medical certificate often includes specific elements such as diagnosis, expected recovery timeline, and recommendations for activity restrictions or return-to-work protocols.
In educational settings, forms designed for absenteeism due to illness adhere to legal frameworks ensuring students’ rights while safeguarding institutional responsibility. Each format includes standardized sections to guarantee clarity and consistency across healthcare providers and institutional gatekeepers.
Structure and Essential Components of Medical Certificate Forms
Every rigorously designed medical certificate follows a common architecture to ensure completeness and usability. Key elements include: - **Patient Identification**: Full name, date of birth, medical record number, and contact details.- **Date and Time of Assessment**: Exact date and time the condition was diagnosed or evaluated. - **Clinical Diagnosis and Symptoms**: Clear, concise medical findings presented in plain but professional language. - **Diagnostic Tests or Treatments**: References to relevant tests, medications, or interventions applied.
- **Functional Limitations**: Specific declaration of activity restrictions, required time off, or precautions (e.g., no lifting over 10 lbs). - **Recommendations and Duration**: Provider’s advice on recovery timeline, follow-up appointments, or workplace modifications. - **Signatory Details**: License number, professional title, and signature of the certifying clinician.
- **Institutional Endorsement**: Space for employer or institution validation, confirming the certificate’s operational use. These components reduce ambiguity, minimize claim denials, and align with requirements across regulatory environments. For example, in the UK’s NHS framework, statutory sickness certificates mandate specific disclosures to prevent misuse while enabling appropriate healthcare access.
Standardization across forms enhances interoperability. In multi-institutional settings—such as large corporations or integrated healthcare networks—uniform format reduces administrative friction and misinterpretations. Digital scoring systems now integrate these templates, automatically validating required fields and flagging incomplete submissions, accelerating processing and reducing human error.
This shift underscores how medical certificate forms have evolved from paper-based artifacts to dynamic digital tools embedded in healthcare systems.
Beyond Paper: The Digital Revolution in Medical Certification
The transformation of medical certificate forms into digital platforms marks a pivotal advancement in healthcare delivery. Electronic health records (EHRs) now support real-time templates, increasing accuracy and enabling data analytics across health systems. A 2023 study in the Journal of Medical Informatics found that digital certificate submission reduced processing time by 68% compared to traditional paper forms, with error rates decreasing by 42% due to automated validation and integrated clinical decision support tools.Digital forms improve accessibility as well. Patients can access electronic templates via patient portals, complete them with supporting documentation, and submit securely—often with built-in prompts for critical fields like diagnosis codes or return-to-work timelines. This patient-centered approach enhances compliance by reducing administrative burden and minimizing the stigma sometimes tied to physical paper submissions.
“Digital adoption doesn’t just streamline workflows—it strengthens trust,” states Dr. Rajiv Mehta, a healthcare informatics specialist. “When patients complete their certificates through intuitive interfaces, they’re more engaged and more likely to provide true, timely information.”
However, the transition raises important considerations.
Data privacy under regulations like GDPR or HIPAA demands robust encryption and access controls. Healthcare practices must ensure platforms meet cybersecurity standards to protect sensitive health data. Furthermore, equitable access remains a challenge—older patients or those with limited digital literacy may struggle without support, necessitating hybrid models that offer phone-based assistance or in-person help at clinics and workplaces.
Regulatory Variance and Global Standards
Medical certificate form requirements differ significantly by country and institution, shaped by local health laws and labor policies. In the United States, for example, workplace medical certifications fall under state-specific workers’ compensation statutes, varying widely in documentation depth and scope. Conversely, European frameworks like those in Germany or France emphasize standardized formats aligned with national insurance schemes, ensuring uniformity across carers and institutions.International organizations such as the World Health Organization advocate for harmonized principles in medical certification—particularly for cross-border mobility and international employment. “Consistency in structure and content across regions facilitates diagnosis verification, insurance claims, and medical validity checks,” explains Dr. Anika Patel, a public health policy expert.
“Standardization supports global health security by enabling reliable, comparable records that transcend linguistic and regulatory boundaries.”
Nonetheless, local customization is essential. Cultural attitudes toward illness disclosure, privacy expectations, and occupational safety norms influence form design and compliance. Successful implementation thus depends on balancing global best practices with local legal and social realities, ensuring medical certificates remain effective, respectful, and enforceable worldwide.
Ethical Dimensions and Professional Integrity
The act of certifying a medical condition carries significant ethical weight. Physicians are bound by codes of medical ethics that prioritize patient welfare, objectivity, and professional accountability. A certificate must reflect true clinical assessment, not external pressure from employers or insurers.“While institutional guidelines provide context, the core responsibility remains clinical truth,” emphasizes Dr. Miriam Chen, an ethics consultant in medical law. “Altering findings undermines trust and risks harm—both to patients and the profession.”
Transparency is key.
Patients deserve clear explanations of why certain restrictions apply, backed by objective medical evidence. Where employment or insurance interests promote repeated certifications, practices must uphold due diligence to avoid overmedicalization. Professional integrity thus shapes not only individual decisions but reinforces the credibility of healthcare as an institution.
Practical Guidance for Clinicians and Institutions
For healthcare providers issuing medical certificates, clarity and precision are non-negotiable. Default templates reduce ambiguity—each section should reflect current clinical knowledge and organizational protocols. Key recommendations include: - Use plain, unambiguous language—avoid jargon unless standardized.- Include specific dates, times, and clinical details to support validity. - Record if remote assessment applies, with supporting telehealth documentation. - Clearly state the duration of invalidation or restrictions.
- Obtain informed consent, explaining how the certificate will be used. - Store records securely, maintaining audit trails for compliance. - Implement digital workflows with validation rules to prevent expedited, incomplete claims.
For employers and institutions, the focus is on consistency and fairness. Establishing clear internal procedures for certificate acceptance, return-to-work timelines, and appeals fosters timely, compliant decisions. Training HR staff to recognize legitimate medical needs—rather than defaulting to skepticism—improves recoveries and workplace morale.
Open communication between providers and organisations ensures clarity, reducing disputes and delays.
Looking Forward: The Evolving Role of Medical Certificate Forms
Medical certificate forms stand at the intersection of medicine, law, and administration—tools that evolve continuously to meet emerging challenges. From digital integration and global standardization to ethical vigilance and patient empowerment, the trajectory points toward greater efficiency, transparency, and trust.As healthcare systems grow more interconnected and patient-centered, these forms remain indispensable: not just bureaucratic checkboxes, but dynamic instruments safeguarding health outcomes and institutional integrity. In an era defined by rapid change, the medical certificate endures as a cornerstone of responsible care, one signed declaration at a time.

Related Post
Navigating Medical Certificate Forms: A Comprehensive Guide for Employers and Employees
Andrade El Idolo Breaks Silence on His Departure from AEW
Rumi Neely Rumi Dowson Biography

Smallest College in the U.S.: A Tiny Institution Tightly Packed with Potential

