Mastering Sepsis: The Critical Role of ICD-10 Code A in Diagnosis and Patient Care
Mastering Sepsis: The Critical Role of ICD-10 Code A in Diagnosis and Patient Care
Sepsis remains one of the most urgent and complex challenges in modern medicine, a life-threatening condition triggered by the body’s overwhelming response to infection. Early recognition and accurate coding—especially using the precise ICD-10 code A—can be the difference between recovery and fatal outcome. This comprehensive guide unpacks the medical, coding, and clinical significance of ICD-10 code A, offering healthcare professionals a clear roadmap for diagnosis, treatment, and vital statistical reporting in sepsis management.
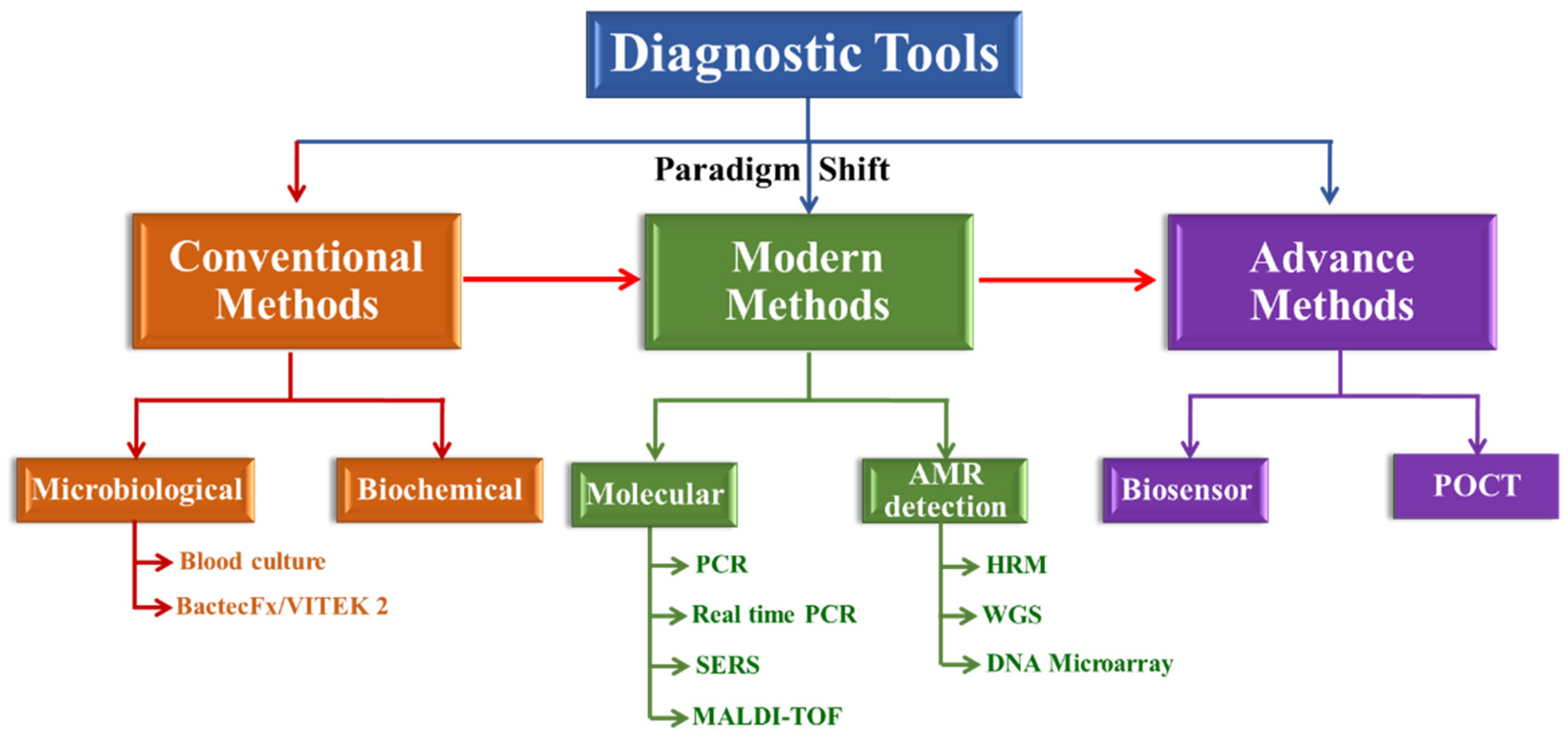
The ICD-10 code A, designated as sepSepsis, is the official diagnostic identifier used globally to document sepsis across electronic health records and billing systems. Codified under the broader category of systemic infections with organ dysfunction, this code enables standardized data collection, crucial for epidemiological tracking, resource allocation, and clinical outcome analysis. According to the World Health Organization, sepsis contributes to nearly 11 million deaths annually, underscoring the imperative for precise coding to guide timely intervention.
Decoding ICD-10 Code A: Definition, Clinical Criteria, and Warning Signs
ICD-10 code sepSepsis refers to sepsis in adults and children presenting with evidence of systemic inflammatory response syndrome (SIRS) triggered by infection, accompanied by measurable organ dysfunction.The clinical definition aligns with two core criteria:
1. The presence of recognized infection—whether localized or systemic—documented through available evidence such as cultures, imaging, or microbiological analysis.
2. At least one organ system demonstrates dysfunction, indicated by abnormal laboratory values (e.g., lactate >2 mmol/L, altered pH, respiratory or renal failure) or clinical signs like hypotension, altered mental status, or oliguria.
Healthcare providers monitor for telltale symptoms including rapid breathing, elevated heart rate, fever or hypothermia, and confusion. “The key is imbalance—normal vital signs do not rule out sepsis,” cautions Dr. Elena Ramirez, Infectious Disease Specialist at Johns Hopkins Medicine.
“Time is tissue,” she emphasizes. “Delays in diagnosing sepsis beyond 6–12 hours significantly increase mortality risk.”
Key adverse markers integrate into clinical assessment: elevated lactate levels (>2 mmol/L) reflect tissue hypoperfusion; acute kidney injury (increased creatinine), respiratory distress (low PaO2 on blood gas), or acute liver dysfunction (elevated bilirubin). These parameters fuel clinical decision-making and determine whether sepsis transitions from suspected to confirmed via clinical criteria such as SOFA (Sequential Organ Failure Assessment) scores.
ICD-10 Code A: Clinical Implications, Treatment Pathways, and Multidisciplinary Coordination
When a diagnosis of sepsis—code A—is confirmed, immediate multidisciplinary response is critical.Treatment begins with aggressive antimicrobial therapy within the first hour of suspicion, tailored to likely pathogens and resistance patterns per local guidelines. Beyond antibiotics, management includes fluid resuscitation, vasopressor support, and organ-specific interventions—such as renal replacement therapy or intubation for acute respiratory failure. “The integration of ICD-10 code A into electronic medical records supports rapid alert systems, enabling early escalation to critical care,” explains Dr.
Malik Chen, Chief Emergency Medicine Physician at a major U.S. healthcare system.
“Codes like sepSepsis trigger real-time notifications to clinicians, Pharmacists, and Infection Control teams, creating a synchronized response.”
ICD-10 code A also underpins quality improvement initiatives and healthcare analytics.
By categorizing sepsis cases consistently, hospitals monitor hospital-acquired sepsis rates, assess delays in interventions like lactate measurement, and evaluate treatment efficacy across patient cohorts. This standardization supports national reporting, clinical research, and public health surveillance efforts—ultimately strengthening public health defenses against one of medicine’s most dynamic threats.
How Healthcare Systems Leverage ICD-10 Code A for Better Outcomes
Healthcare institutions increasingly rely on precise sepsis coding to drive clinical decision support and optimize workflows. Integrated EHR systems flag code A-based alerts at point of care, prompting timely sepsis screening using validated tools like the Sepsis-3 definition.Dashboards display real-time metrics: time from admission to antibiotic administration, source control interventions, and survival rates. These data feed performance metrics, guide protocol refinements, and ensure compliance with national sepsis campaign benchmarks. Initiatives like the U.S.
Centers for Disease Control and Prevention’s “Get Sepsis Smart” campaign highlight the importance of standardized coding. “ICD-10 codes transform anecdotal experience into data-driven insight,” notes Dr. Priya Rao, Clinical Data Scientist at a leading health system.
“They make sepsis visible, measurable, and manageable across care settings.”
The Future of Sepsis Coding: Precision Medicine, AI, and Beyond As medicine advances, ICD-10 code A evolves beyond a diagnostic label into a portal for precision interventions. Emerging technologies enable risk stratification through machine learning models trained on coded patient data, predicting sepsis onset before clinical signs manifest. Natural language processing refines automated coding accuracy, reducing errors in real-world application.
Despite technological strides, clinical judgment remains paramount. “No algorithm replaces a trained eye,” affirms Dr. Chen.
“Codes guide, but clinicians drive outcomes.” The convergence of structured ICD-10 coding and clinical expertise forms the backbone of sepsis care evolution—one where standardized data fuels innovation, lifelong learning, and improved survival.
In sum, ICD-10 code A is more than a diagnostic marker; it is a vital thread weaving together clinical practice, public health strategy, and medical research. Its proper use enables faster diagnosis, coordinated treatment, and actionable data that transforms sepsis management from reactive to proactive.
As frontline providers harness the full potential of ICD-10 classification, they illuminate a path toward saving lives, one sepsis case at a time.


Related Post
Jelly Roll Makes Surprise Cameo During 1127 WWE RAW
Comprehensive Guide to Alyx Star: Bio Insights and Personal Details That Define a Digital Icon
Cassandra Freeman Movies Bio Wiki Age Husband and Net Worth

Mike Rowe’s Relentless Call: What America’s Skilled Trades Teach Us About Pride, Pay, and Purpose

