Ipratropium Bromide: Not a Steroid, but a Key Player in Respiratory Therapy — Here’s What You Need to Know
Ipratropium Bromide: Not a Steroid, but a Key Player in Respiratory Therapy — Here’s What You Need to Know
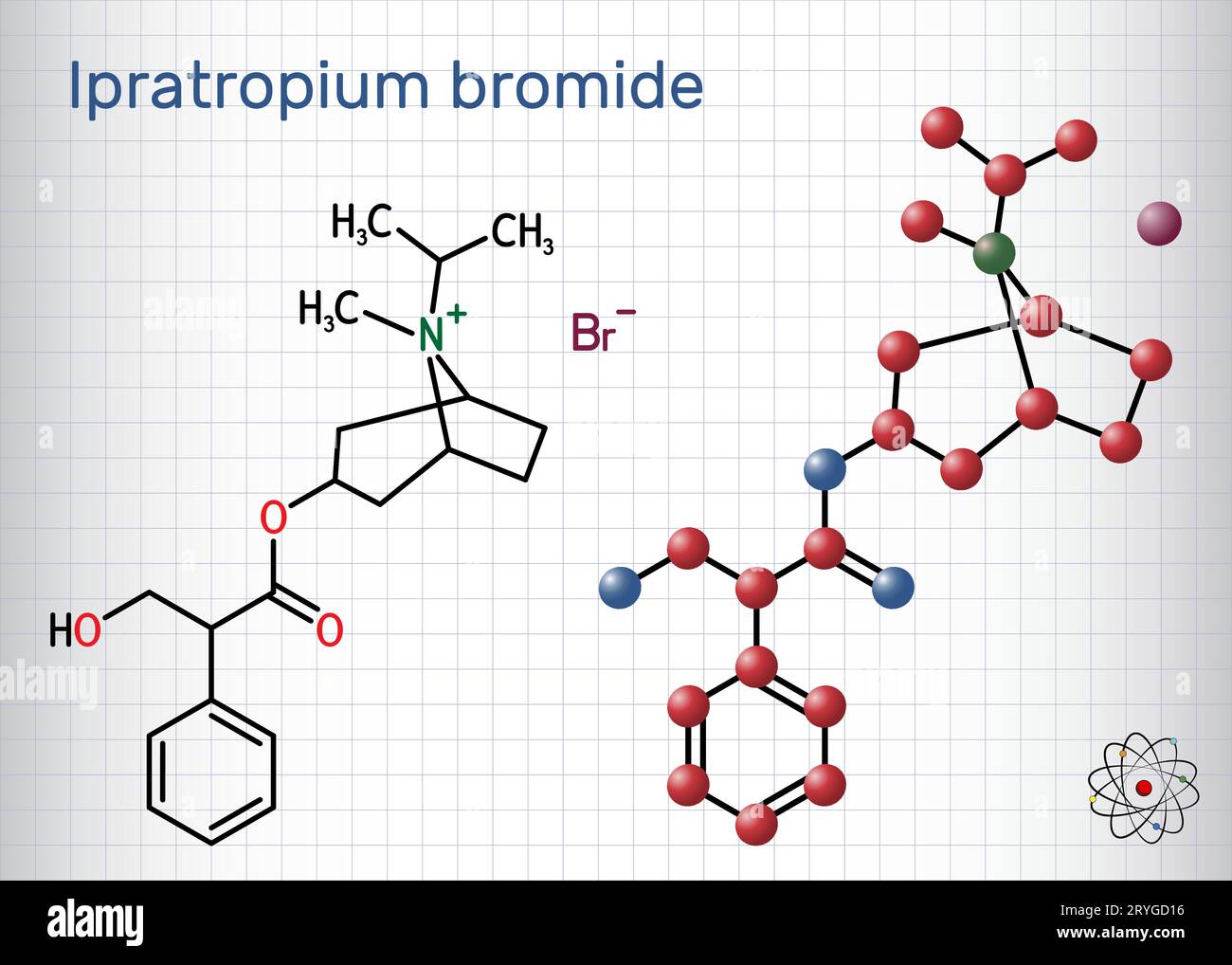
Ipratropium bromide stands apart in the landscape of respiratory medications, often mistaken for a steroid due to its potent anti-inflammatory benefits in treating chronic obstructive pulmonary disease (COPD) and asthma. Yet, unlike corticosteroids, it operates through a distinct mechanism—targeting muscarinic receptors to relax bronchial muscles—making its role in breathing control both unique and vital. While not a steroid, the drug shares therapeutic goals with steroid-based treatments: reducing symptoms, improving airflow, and enhancing quality of life.
Understanding its true nature is essential for patients, providers, and anyone navigating respiratory care.
The Misclassification: Ipratropium Bromide and Its Pharmacological Identity
Despite frequent confusion, ipratropium bromide is not a steroid. It belongs to a class of medications known as anticholinergics, specifically "long-acting antimuscarinic agents" (LAMAs).Steroids, such as fluticasone or budesonide, work by dampening systemic and local inflammation, but ipratropium’s mechanism diverges significantly. It blocks acetylcholine receptors in the airway smooth muscle, preventing contraction triggered by autonomic nerve signals. This action leads to bronchodilation—widening airways—without suppressing immune responses.
“The key distinction lies in how each class treats airflow obstruction,” explains Dr. Elena Torres, pulmonologist and steroid therapy expert. “Corticosteroids reduce underlying inflammation and prevent flare-ups, while ipratropium provides immediate muscle relaxation for sustained relief during exacerbations or daily symptom management.” This functional difference underscores why clinical guidelines distinguish between steroid use and anticholinergic therapy.
Mechanism of Action: How Ipratropium Helps Breathe Easier At the cellular level, ipratropium bromide exerts its effects by targeting M3 muscarinic receptors located on bronchial smooth muscle. Normally, acetylcholine—released during nervous activation—triggers contraction, narrowing airways and causing breathing difficulty. By competitively blocking these receptors, ipratropium prevents this contraction, promoting sustained bronchodilation.
Unlike beta-agonists that stimulate disensitive nerves, ipratropium’s action is receptor-specific, offering a complementary mechanism in respiratory therapy. The drug’s long duration—up to 12 hours—makes it ideal for once- or twice-daily use, maintaining airway openness without frequent dosing. This pharmacokinetic profile contrasts with many inhaled steroids, which require daily administration and work best when paired with bronchodilators.
When administered via metered-dose inhalers or dry powder inhalers, ipratropium reaches the lungs efficiently, with minimal systemic absorption, reducing the risk of steroid-like systemic side effects such as osteoporosis or adrenal suppression.
Clinical Use: Where Ipratropium Shines in Respiratory Care
Ipratropium bromide is a cornerstone in the management of two primary respiratory conditions: COPD and asthma. In COPD, where airway inflammation and chronic bronchoconstriction dominate, the drug serves as a backbone in rescue and maintenance regimens.It is frequently combined with short-acting beta-agonists (SABA), such as albuterol, in fixed-dose inhalers, offering synergistic effects—immediate relief paired with prolonged action. For asthma, particularly in patients with featured cholinergic hyperresponsiveness, ipratropium enhances symptom control. Clinical trials, including studies published in the Journal of Allergy and Clinical Immunology, show that asthma patients who add ipratropium experience fewer exacerbations, reduced airflow obstruction, and improved peak expiratory flow rates when combined with inhaled corticosteroids.
Beyond COPD and asthma, ipratropium finds niche use in bronchiectasis, where mucus clearance is impaired. Its bronchodilatory effect facilitates expectoration, reducing infection risks. The drug’s role in preventing exercise-induced bronchoconstriction and nocturnal symptoms further broadens its clinical applicability.
Safety Profile: A Favorable Alternative to Steroids One of ipratropium bromide’s strongest attributes is its superior safety profile compared to inhaled corticosteroids. While steroids carry long-term risks like thrush, hoarseness, adrenal modulation, and bone density loss—with minimal systemic absorption in proper use—anticholinergics like ipratropium are generally well-tolerated. Common side effects include dry mouth, throat irritation, and urinary hesitation—effects tied to its muscarinic blockade in peripheral tissues.
“Patients often worry about sedation or weight gain with steroids, but those concerns are not shared with ipratropium,” notes Dr. Rajiv Mehta, a clinical pharmacologist specializing in inhaled therapies. “Most adverse events are mild and self-limiting, especially with proper device technique and rinsing oral tissues after use.” Notably, in elderly patients with age-related cognitive decline, prolonged use of un-rinsed anticholinergics may increase dementia risk.
However, when used short-term or as prescribed for specific conditions, ipratropium remains a safe option. The drug’s mechanism spares the immune system, making it an attractive choice for those needing non-steroidal pulmonary support.
Comparing Ipratropium to Steroids: Bridging Gaps in Respiratory Therapy Where steroids reduce inflammation, ipratropium eases obstruction—two complementary strategies in respiratory medicine.
While steroids prevent goblet cell hyperproduction and airway remodeling, anticholinergics offer immediate mechanical relief by lowering baseline airway resistance. This synergy is codified in global guidelines, such as those from GINA (Global Initiative for Asthma) and GOLD (Global Initiative for Chronic Obstructive Lung Disease), where combination therapy is routinely recommended. For example, the GOLD 2023 report emphasizes: “In moderate-to-severe COPD, adding a long-acting anticholinergic like ipratropium to LABA therapy significantly improves symptom control when stat therapy is insufficient.” Such endorsements reflect how ipratropium fills a critical gap in first-line treatment, especially for patients unresponsive or intolerant to steroids alone.
Moreover, in acute exacerbations, ipratropium administered via nebulizer or inhaler delivers rapid symptom relief without steroid-related side effects, supporting its role in both prevention and crisis management. Its compatibility with other controller drugs—steroids, leukotriene modifiers, phosphodiesterase inhibitors—further enriches treatment flexibility.
Patient Experience: Real-World Impact and Satisfaction Patient-reported outcomes reveal ipratropium’s positive impact on daily living.
A 2022 survey by the COPD Foundation found that 82% of users rated symptom relief from ipratropium-based therapy as “significant” or “very significant,” with reduced wheezing, shortness of breath, and nocturnal awakenings. Many noted improved exercise tolerance and reduced dependency on rescue inhalers. For asthma patients, qualitative interviews highlight reduced anxiety around sudden bronchospasm.
“Knowing I’ve a reliable bronchodilator gives me confidence,” said one respondent. “I still use my steroid inhaler, but i



Related Post
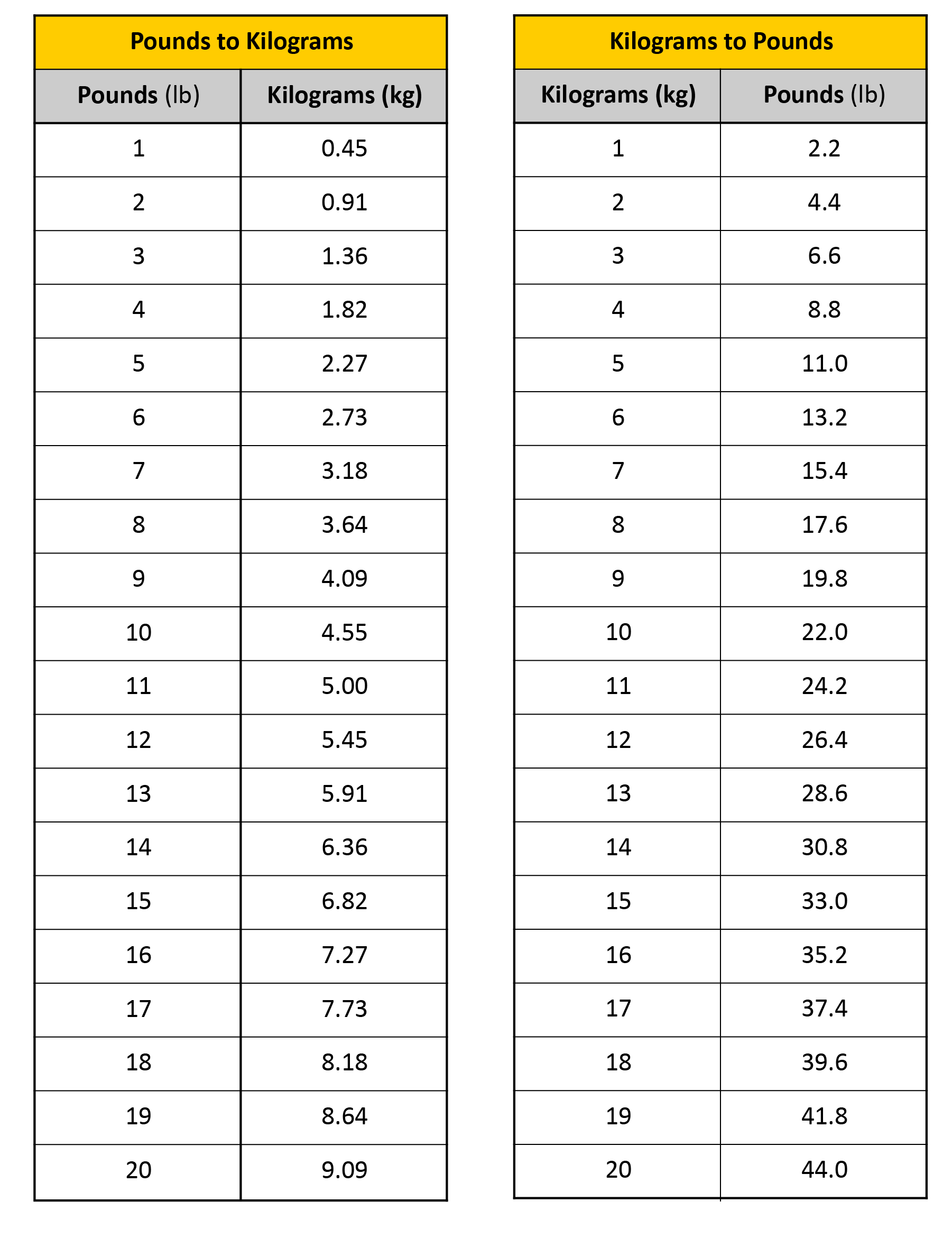
How 11,000 Grams Translate: The Definitive Guide to Converting Kilograms to Pounds for Global Accuracy
Alexa Bliss Loved Beating Randy Orton Thanks To Fire Coming Out Of Her Hands