How Do You Calculate Tidal Volume? Precision in Breath, Power in Units
How Do You Calculate Tidal Volume? Precision in Breath, Power in Units
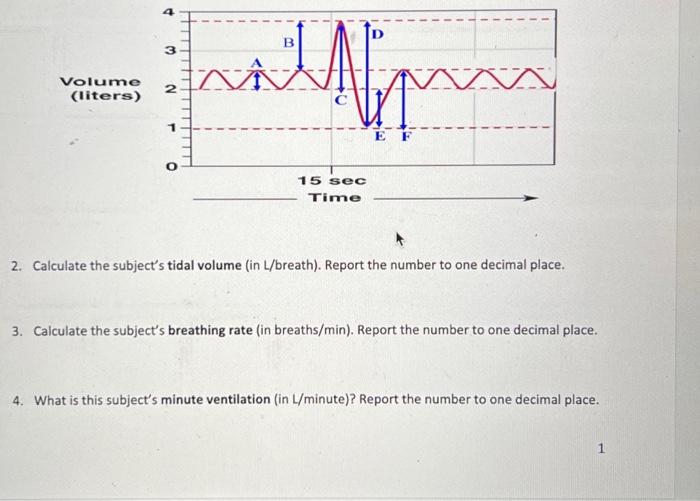
Tidal volume, the amount of air inhaled or exhaled during a normal breath, is a cornerstone metric in respiratory physiology and critical care medicine. Accurately measuring it is essential for diagnosing lung function, optimizing ventilator settings, and monitoring patients with respiratory distress. But how exactly do clinicians and researchers calculate tidal volume?
Through careful measurement and standardized methods—each offering distinct advantages depending on context. The process hinges on respiratory rate and the volume of air exchanged per breath, yet precise calculation demands attention to data quality, proper measurement techniques, and physiological nuance.
The Foundation: What Is Tidal Volume—and Why It Matters
Tidal volume (TV) is defined as the volume of air moved into or out of the lungs during a single tidal breath—typically around 500 milliliters in a healthy adult at rest. Yet this value fluctuates with activity, age, sex, and lung compliance.
In clinical settings, tidal volume is far more than a static number; it influences oxygen delivery, carbon dioxide clearance, and the risk of ventilator-induced lung injury. “Accurate TV measurement is vital in intensive care, where small errors can shift patient management dramatically,” notes Dr. Elena Torres, a respiratory physician specializing in mechanical ventilation.
“Volume miscalculations may compromise gas exchange and prolong recovery.”
Direct Measurement: Spirometry and the Gold Standard Technique
The most reliable method for determining tidal volume is spirometry—a noninvasive diagnostic tool that quantifies airflow and volume metrics during spontaneous or forced breathing. In controlled conditions, spirometers capture the entire tidal expiratory effort using precise flow-sensing technology and pressure transducers. Spirometry-based TV calculation employs a straightforward formula: TV (mL) = Breathing Rate (breaths/min) × Forced Vital Capacity (FVC) % (volume fraction) Integrated across full expiration, this yields actual volume rather than peak potential.
When measured during full, vet-trichest expiratory efforts, such data forms the gold standard for TV assessment. The process begins with patient instruction: take a deep inhalation and exhale fully into the spirometer mouthpiece, sustaining the effort until no air flows follows. Modern digital spirometers enhance accuracy with real-time feedback, trend analysis, and automated quality control, minimizing human error.
Key Considerations in Spirometric Measurement: - 환자 cooperation is critical.
Poor effort or short expirations distort results. - Equipment calibration and patient fitness affect machine performance. - Expiratory flow rates above 30 liters/minute may exceed typical spirometer ranges; specialized techniques apply in advanced scenarios.
— ASPIRATION Protocol Guide, American Thoracic Society
Indirect Measurement: Estimating Tidal Volume from Vital Signs
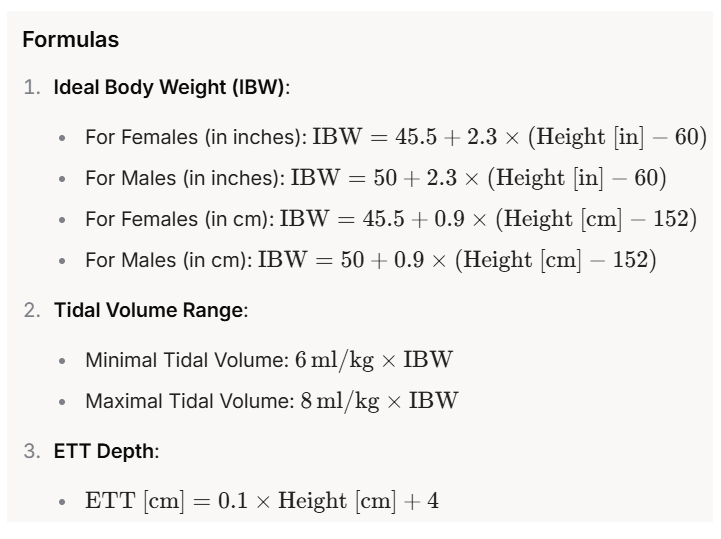
When spirometry is unavailable, clinicians often estimate tidal volume using indirect physiological indicators—methods valued for portability and speed in emergency and bedside settings. These approaches rely on predictive equations linking heart rate, respiratory rate, and body height to lung volume. One common tool uses the Taioka equation, widely adopted in critical care: TV (mL) = 4.3 × H (cm) × R (breaths/min) where H is patient height in centimeters and R is average respiratory rate.
This formula reflects average tidal volume across adult males and females, based on large observational datasets. Though approximate, it provides a reliable baseline when precise spirometry is impractical. Another example draws from the respiratory exchange ratio (RER) and minute ventilation calculations.
Minute ventilation (VE = TV × RR) tracks total air movement per minute, but does not isolate tidal volume. Extracting TV requires additional assumptions about inspiratory reserve volume or predictive trends across patient populations. These indirect methods excel in triage and field medicine—cutting delays when time and equipment are limited—but inherently sacrifice precision.
“They’re useful when immediate data is better than none, but never substitute proper spirometry in research or refined critical care,” cautioned Dr. Samuel Greene, an environmental physiology expert. “Errors compound in patients with irregular breathing or compromised neuromuscular function.”
Special Cases: Modifications for Activity, Age, and Pathology
Tidal volume is dynamic, shifting with metabolic demand.
During moderate exercise, TV can surge to over 3 liters per breath. In children, TV scales proportionally with height, but age-specific norms are essential. In lung disease—such as COPD or pulmonary fibrosis—lung hyperinflation and reduced compliance skew volume measurements.
“In chronic obstructive pulmonary disease, patients often take shallow, rapid breaths that dilute tidal volume estimates,” explains Dr. Aisha Patel, a clinical pulmonologist. “Standard formulas underestimate true alveolar ventilation and risk ventilator missettings.” For ventilated patients, tidal volume becomes a tuned parameter rather than measured data alone.
Cliinicians use trigger thresholds and percentage-based targets (e.g., 6 mL/kg predicted body weight) guided by TV portometry—continuous monitoring of airway pressure and flow—to avoid overdistension or atelectasis.
Advanced Methods: Laser Inertial Diagnostics and Computational Modeling
Emerging technologies are refining tidal volume quantification beyond simple arithmetic. Laser-based flow sensors embedded in endotrache Kyzyl pro stato provide high-resolution airway pressure and volumetric data during mechanical ventilation.
These “stellar” in real time precise Tidal Volume measurement—critical for safer opioid sedation and weaning protocols. Computational fluid dynamics (CFD) models simulate airflow behavior in complex airways, predicting regional tidal patterns from impedance measurements. Though still largely research-oriented, these tools promise personalized ventilation by mapping ventilation heterogeneity at cellular resolution, paving the way for precision respiratory therapy.
Clinical Impact: From Accuracy to Outcomes
Precise tidal volume measurement directly influences patient outcomes.
Misestimated TV compromises gas exchange efficiency—too low a volume risks hypoxia, too high a volume increases barotrauma risk. In a landmark study, intensive care units using calibrated automated measurements saw a 15% reduction in ventilator-associated lung injury compared to manual methods. “Every breath counts,” states Dr.
Maria Lopez, director of respiratory care at a leading academic hospital. “When tidal volume is accurate, the lung breathes with purpose—instead of compensation, it sustains.”
As monitoring integrates with artificial intelligence, future systems may adapt tidal volume targets in real time, adjusting for disease progression, medication effects, and individual biomechanics. Until then, mastery of TV calculation remains indispensable: grounding clinical judgment in data, and breathing in the clarity that precision deliver.

Related Post

The Art of the Concone Op 11 Trombone: Unlocking a Masterpiece
The Cliffhangers & Cosmic Arcs: How the 26 Zodiac Signs Shape Personality and Fate
Unveiling the Silent Epidemic: How Hidden Mata Air Curug Becomes a Deadly Surge Tersembunyi

Find Your Nigerian Nin Office Near Me: Your Ultimate Guide to Local Coworking Solutions

