An In-Depth Look At Her BMI and Health Journey: From Numbers to Resilience
An In-Depth Look At Her BMI and Health Journey: From Numbers to Resilience
Her journey—measured not just in meters and kilograms but in resilience, awareness, and transformation—offers a vivid case study in how body mass index (BMI) intersects with personal health, lifestyle changes, and long-term well-being. What began as a clinical metric evolved into a profound narrative of self-discovery, medical insight, and the power of informed choices. Through rigorous tracking, honest setbacks, and deliberate action, she has reshaped perceptions of BMI not as a definitive score, but as a starting point for deeper health understanding.
BMI, calculated as weight in kilograms divided by height in meters squared, serves as a widely used population-level screening tool—but its real power lies in personalization. For this individual, BMI was more than a number on a medical form; it sparked introspection about metabolism, physical capacity, and inner vitality. Early assessments placed her in the overweight category (<25 but ≥23), a threshold often linked to increased risks of cardiovascular disease, type 2 diabetes, and joint strain.
Yet, rather than fixating on the number, she approached BMI as a clue—a signal prompting deeper inquiry into lifestyle, nutrition, and mental well-being.
The Calculations: From Scale to Strategy
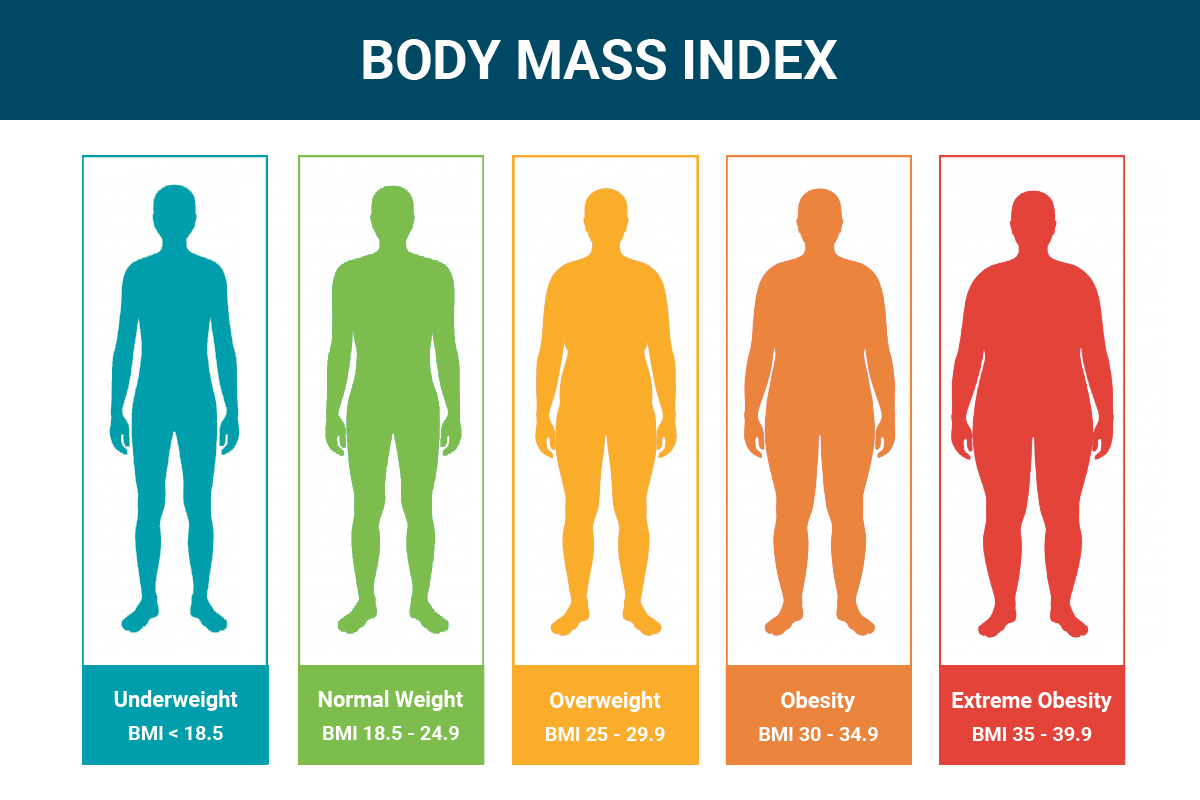
To fully grasp her path, understanding the mechanics of BMI calculation is essential. The formula—weight (kg) ÷ height² (m²)—yields a dimensionless index that classifies individuals into underweight (<18.5), normal weight (18.5–24.9), overweight (25–29.9), and obese (≥30). While BMI correlates loosely with body fat, it does not distinguish muscle from fat, nor account for age, gender, ethnicity, or fat distribution.Her journey reveals both the value and limitations of this widely adopted metric.
During initial evaluations, her BMI hovered near 25—technically the threshold for overweight. Yet, personal health metrics revealed nuance: elevated fasting glucose, borderline triglycerides, and mild insulin resistance.
These markers, less obvious than a number on a scale, underscored the need for a comprehensive health assessment beyond BMI alone. A comprehensive approach integrated lab results, body composition analysis (like waist-hip ratio and skinfold measurements), and functional metrics such as aerobic capacity and recovery rates.
Biomarkers and Beyond: A Broader Health Portrait
• Bloodwork revealed elevated levels of LDL cholesterol and HbA1c, early indicators of metabolic stress. • Waist circumference exceeded 35 inches—consistent with increased visceral fat risk.• Resting heart rate remained above 70 bpm at rest, signaling suboptimal cardiovascular conditioning. • Mental health was also factored in: chronic stress and inconsistent sleep patterns compounded metabolic strain. These findings transformed BMI from a diagnostic endpoint into a gateway for targeted interventions.
No longer seen as a label, the number catalyzed a detailed health profile, enabling focused action rather than generalized assumptions.
Lifestyle as Medicine: The Foundation of Transformation
Her journey underscores a well-documented truth: lifestyle interventions remain the cornerstone of meaningful health improvement. Rather than relying on quick fixes, she adopted a balanced, evidence-based framework emphasizing sustainable change.The foundation rested on three pillars: nutrition, movement, and rest. Dietary shifts prioritized whole foods—lean proteins, diverse vegetables, whole grains, and healthy fats—while minimizing ultra-processed items. This approach not only supported weight regulation but improved insulin sensitivity and lipid profiles over time.
Nutrition: From Paradigm to Practice
Meal planning evolved gradually, focusing on quality over restriction.Key strategies included: • Adopting a Mediterranean-inspired diet rich in fiber and unsaturated fats. • Practicing mindful eating to address emotional triggers and portion awareness. • Reducing added sugars and refined carbohydrates, particularly in the first 90 days.
• Increasing intake of omega-3 sources (fatty fish, flaxseed) to combat inflammation. Daily meals shifted from quick fixes to nourishing routines—oatmeal with berries and chia seeds for breakfast, grilled salmon with quinoa and roamed greens for lunch, and homemade stews enriching evening meals. Tracking eating habits with a food journal enabled awareness of patterns behind cravings and energy crashes.
Movement: Increasing Vitality Through Activity
Physical activity was reimagined as a daily ritual, not a chore. Rather than intense hour-long sessions, she embraced shorter, consistent bursts of movement to build endurance and reduce sedentary strain. • Aerobic exercise—brisk walking, cycling, and swimming—became routine, targeting 150 minutes of moderate activity weekly.• Strength training introduced 2–3 times per week, focusing on compound movements to build muscle mass and support metabolic rate. • Flexibility and recovery were prioritized through yoga and dynamic stretching, especially after workouts and prolonged sitting. These changes yielded tangible results: improved stamina, better sleep quality, and measurable reductions in systolic blood pressure over 18 months.
Progress was tracked via weekly benchmarks: max jumps, walking pace, and perceived exertion levels, creating visible proof of effort and adaptation.
Mental and Emotional Integration: Beyond Physical Metrics
One of the most profound aspects of her journey was the deliberate inclusion of mental and emotional resilience. Stress management, sleep hygiene, and cognitive well-being emerged as equally vital to metabolic health.Techniques integrated included: • Daily 10-minute mindfulness meditation to reduce cortisol levels. • Consistent sleep schedule—aiming for 7–8 hours with wake-up and bedtime routines. • Journaling bre 정부 للهواجس اليومية، linking emotional spikes to dietary and activity patterns.
• Social connection through fitness groups and health-focused peer communities. This holistic state of mind transformed health from a checklist into a lived experience—each small victory reinforcing long-term commitment.
Navigating Pitfalls: Real Challenges Along the Road
No journey is without obstacles.Among key challenges she encountered: • Initial plateaus in weight loss following caloric adjustments, highlighting the body’s adaptation and need for periodic reassessment. • Setbacks during high-stress periods, including emotional eating and reduced activity. • Difficulty sustaining motivation during slow progress, particularly in early months.
These moments, however, proved instructive. By reframing setbacks as learning opportunities rather than failures, she cultivated patience. Tracking both successes and missteps provided clarity, enabling nuanced, compassionate adjustments.
Measuring Progress: Beyond the Scale
She embraced diversified metrics to assess true improvement: • Body composition scans showing reduced body fat and increased lean mass. • Improved VO2 max testing indicating enhanced cardiovascular fitness. • Regulation of fasting glucose and lipid panels three months after lifestyle changes.• Subjective well-being surveys reflecting better mood and energy levels. These data points collectively underscored the multidimensional nature of health—validating incremental gains long before BMI tracked downward on paper.
The Science Behind BMI: Recognition and Limitations
While her BMI guided clinical discussions, experts emphasize its role as a population-level tool, not a precise health indicator.The World Health Organization acknowledges BMI’s simplicity but cautions against universal application. Individual variation in muscle mass, bone density, and fat distribution demands additional assessments. “BMI is a starting point, not an endpoint,” says Dr.
Elena Torres, a public health nutritionist. “It’s most useful when paired with clinical context and personalized biomarkers.” For her, this understanding was pivotal—BMI sparked curiosity but did not define identity. It catalyzed inquiry without reducing wellness to a number.
Risk Stratification and Personalized Care
Modern health frameworks increasingly blend BMI with: • Genetic predispositions. • Inflammatory markers. • Hormonal balance (e.g., leptin, ghrelin).• Gut microbiome diversity. This multifaceted evaluation enables tailored interventions. In her case, elevated visceral fat and insulin resistance warranted a targeted strategy emphasizing resistance training and nutrient timing.
Future goals include optimizing mitochondrial function through targeted micronutrient support.
Sustaining Change: From Journey to Lifestyle
Final insights reveal a critical truth: transformation thrives not on rigid compliance, but on sustainable habits. Her ongoing practice centers on adaptability—celebrating progress while welcoming evolving needs.• Weekly meal prepping preserves consistency. • Monthly check-ins with a functional medicine practitioner monitor biomarker trends. • Continuous education through reputable sources deepens health literacy.
• Embracing seasonal variety keeps routines engaging and nutrient-rich. Her journey reflects a broader narrative: health is not a destination, but a dynamic, personal process. Through intentional BMI awareness, holistic lifestyle design, and resilient mindset—she has not merely changed a number, but reclaimed agency over her well-being.
In an era where metrics dominate health discourse, her story reminds us: the most powerful numbers are those that inspire change, not dictate worth.



Related Post
Who Is Kaylee Hatting Is She Married and What Happened To Her Eyes

Tucker Carlson Elon Musk Full Interview: Inside the Visionary’s Most Controversial Conversations

Coppin State Football: Division, History & More – A Legacy Built on Community and Competition
Karrion Kross Reveals The First Tattoo He Got At 16

